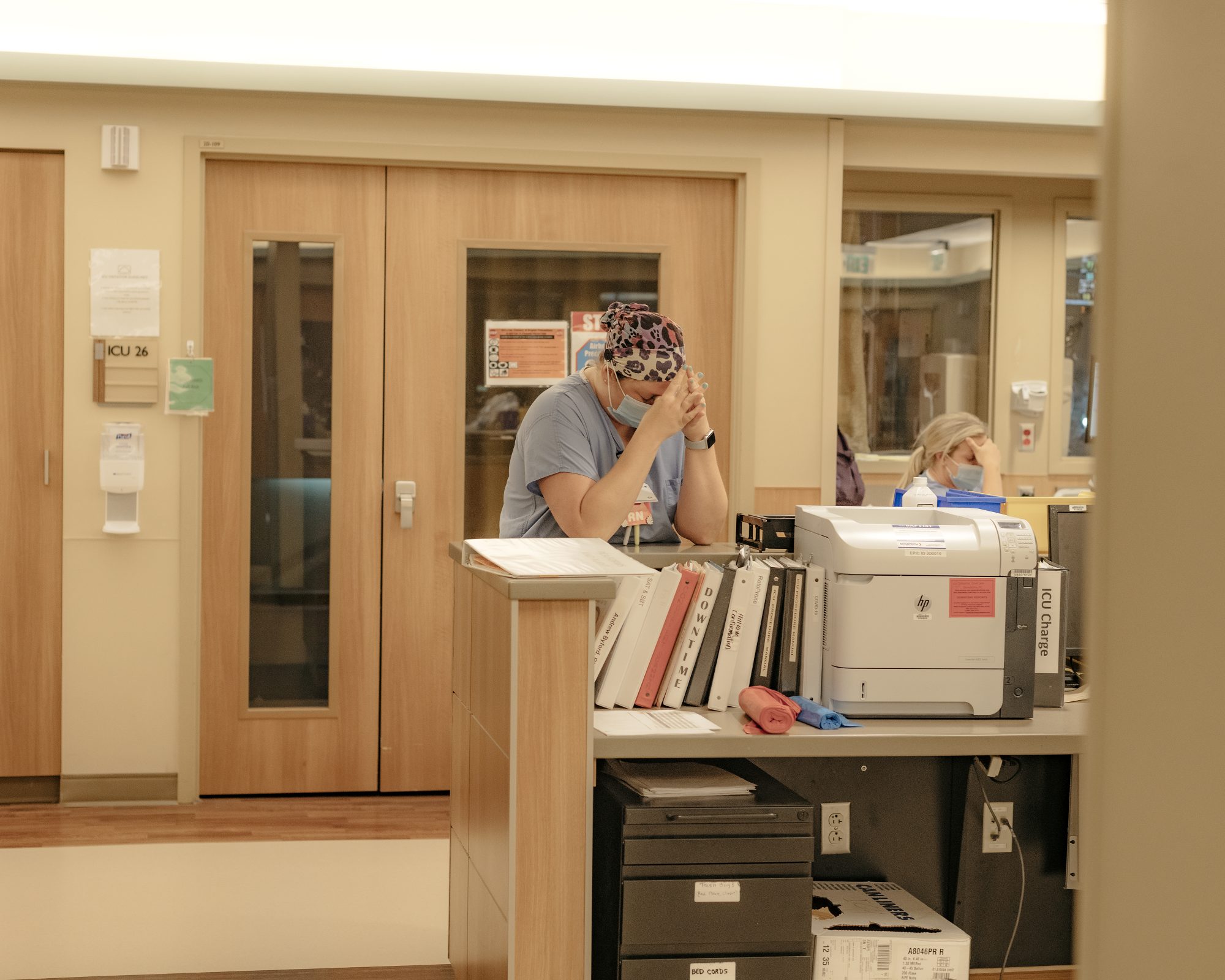
Alexandra Flodin, a 34-year-old intensive care unit nurse in Rockford, Illinois, has three kids between ages 2 and 9. She's been a nurse for 11 years. For most of her nursing career, Flodin was a cardiac nurse but moved to the intensive care unit amid the pandemic. "I've not known an ICU before COVID," she says. "Nurses are getting burned out because we're working more than our required shift."
Across the U.S., hospitals are overburdened with COVID-19 cases and not enough resources. Several states have fewer than 10 percent of ICU beds available, and many more have had to plan to limit and ration the care they can give to all patients.
"We need about eight to nine nurses on a daily basis to staff the unit, and we normally have like four or five," says Flodin.
According to the CDC, there aren't enough health care workers in U.S. hospitals to handle the more than 11,000 COVID-19 hospital admissions that, on average, occur daily in the U.S. Nursing shortages in particular started before the pandemic overwhelmed hospitals. A 2018 study in the journal American College of Medical Quality predicted a shortage of 510,394 registered nurses by 2030. Between the increase in hospitalizations as the Delta variant surges and a child care crisis that has hit health care workers especially hard, the pandemic has exacerbated an already alarming situation for nurses who parent.
The Unequal Load at Home and Work
Even when there isn't a pandemic, balancing a family and life as a health care worker can be challenging. Flodin regularly works twelve-hour shifts, often working three twelve-hour days in a row. Because of the high cost of child care in the U.S., she doesn't mind. "If I had to put my kids in daycare five days a week, it would cost me three times my mortgage," she says. "I choose to work three days a week, so I only need three days of childcare."
That's a benefit of long shifts, says Flodin, but she worries that she missed out on many important events in her children's lives. "It makes me sad that I can't watch my daughter at her dance classes and that I can't enter the school building or the daycare center," she says, explaining that because of her work in a hospital, she has to minimize the exposure of COVID to children in these settings.
"I haven't stepped foot in my son's daycare for a year and a half, but our relationship is good, and I don't think that has changed. We're just living a different way," she says.
Kathryn Konrad, a nursing professor at the University of Oklahoma, says one reason moms are leaving nursing is the gender imbalance in the field and at home. "Nursing is mostly women, so we have a lot of people who just can't balance it anymore," she says. "They have kids at home or older family members at home. They're looking for other opportunities to take care of their family."
Double Duty for Nurses
It's not just the nurses who are in short supply. Leslie Abla, an ICU nurse in Oklahoma City, Oklahoma, says the main issue with staffing on her unit is the supporting and administrative staff. Often the unit doesn't have someone to answer the phones, which then falls on the lead nurse. Her department is also supposed to have two techs, but they usually only have one or sometimes none. The nurses are doing the work of the techs.
"We have to do our baths by ourselves or grab another nurse to help us," Abla says. Many tasks, such as safely turning patients onto their stomach when they're doing poorly, require at least four hospital staff.
Abla's kids are 12 and 16, so they are vaccinated for this current surge. Her husband retired early from his own nursing job to manage the home. Her stress doesn't come from worrying about her children getting sick or from figuring out child care. Before she became a nurse, she was a stay-at-home-mom, so it's been difficult for her to give a lot of those responsibilities over to her husband. She says she continued to do the majority of the household management until recently.
"This year, I decided that I needed to take a hands-off approach," she says. Abla made sure the school included her husband on emails regarding school work and other communications from teachers. "I do recognize that part of it is letting go," she says.
The Mental Burnout
Flodin says the increased hours she's been working at the hospital have negatively impacted her mental state. "I sometimes feel very depressed, and I don't know why. That's different for me. I'm usually very outgoing," she says. "I'm just burnt out, and I bring that home with me."
Unfortunately, she worries her kids have felt the effects of her burnout. "I don't want to go to the park. I don't want to go to the apple orchard because I have to work tomorrow," she says. There's also the increased fear that her line of work could put her family's health in jeopardy.
"Earlier we were worried about bringing COVID home to our families," she says. "Now, we can protect ourselves better, and we're vaccinated, but it's still in the back of our minds."
With demanding workloads at home and in hospitals, nurses who are parents carry a heavy mental burden. The nursing shortage not only increases burnout but reduces patient care quality and increases suicide risk among female nurses—both dire outcomes with no clear end to the pandemic in sight.
If you or someone you know is considering suicide, contact the National Suicide Prevention Lifeline at 800-273-8255, or the Crisis Text Line at 741741 (text HOME). For those struggling with other mental health issues, the National Alliance on Mental Illness offers mental health education, resources, and a helpline (800-950-6264).